Indications for use.
Treatment of acute chronic pain. Analgesic in oncology.
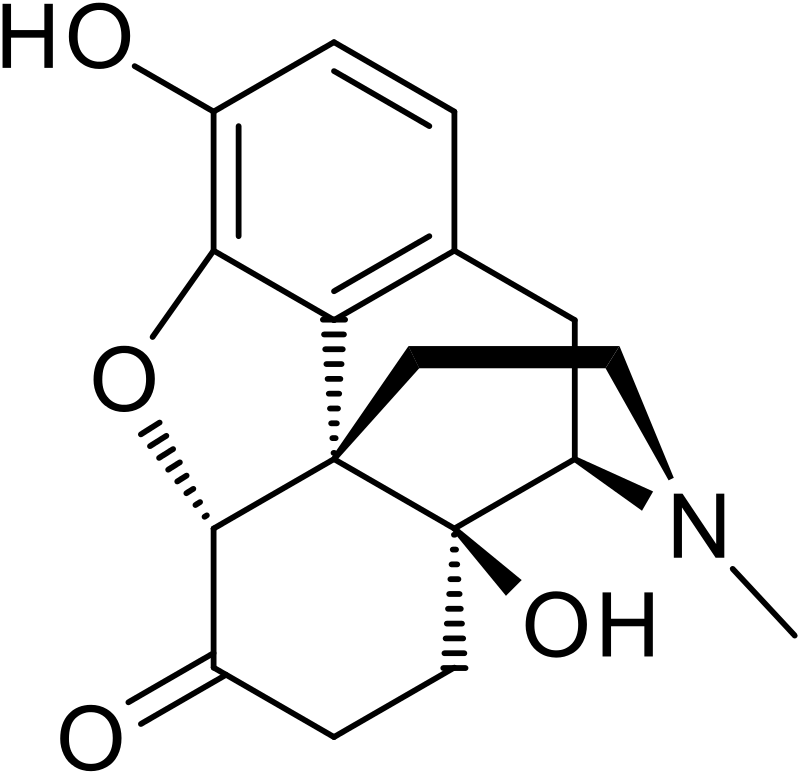
With parenteral administration, Oxymorphone (Oxymorphone, Numorphan) is about 10 times more active than morphine. There is a rapid development of drug addiction and a weak release of histamine. Otherwise similar to morphine.
Method of administration and dosage.
Analgesia: subcutaneously / intramuscularly 0.5 – 1.5 mg 4 – 6 hours. Intravenously 0.5 mg 4 – 6 hours. Rectally 5 mg 4-6 hours. Due to a violation of elimination, accumulation and excess of sedation may be observed in patients with renal or hepatic dysfunction. Analgesia can be increased by additional administration of other narcotic drugs, antidepressants, NSAIDs and non-drug therapy. Elimination: in the liver, kidneys.
Pharmacology.
Oxymorphone has a slight antitussive effect. However, taking oxymorphone may be accompanied by nausea and vomiting more often than morphine. 1 mg of intramuscular oxymorphone is equivalent in analgesia efficiency to 10 mg of intramuscular morphine sulfate. Oxymorphone penetrates the placental barrier and can have a negative effect on fetal development. The drug is excreted from breast milk and should be used with precautions in nursing mothers.
Pharmacokinetics.
Onset of action: intravenously 5-10 minutes; subcutaneously / intramuscularly 10-15 minutes; rectally 15 -30 minutes. Maximum effect: intravenously / intramuscularly 30-60 minutes. Duration of action: intravenously / intramuscularly / subcutaneously / rectally 3-6 hours. Interaction with other medicinal substances. Enhances the central nervous system and the circular effects of a depressant when taking other narcotic analgesics, energy-dependent anesthetics, phenothiacins, sedatives, sleeping pills, alcohol, tricyclic antidepressants; analgesia increases and prolongs when using narcotic and non-narcotic analgesia, for example, aspirin, acetaminophen, clonidine; serological levels and toxic effects increase when taking carbamazepine; liver metabolism increases, and the effectiveness of oxycodone decreases in smokers.
Toxicity:
The toxic range is not always controlled.
Symptoms of intoxication.
Drowsiness, coma, respiratory arrest, asphyxia, cardiac arrhythmia, respiratory and metabolic acidosis, vascular insufficiency, cardiac arrest, death. Antidotes. Naloxone 0.4 – 2 mg intravenously; repeat the dose every 2-3 minutes to a maximum of 10 – 20 mg.
Treatment of complications and poisoning. Stop the administration of the drug, ensure adequate ventilation and blood circulation (airway patency, oxygen therapy, intravenous rehydration, vasopressors); introduce an antidote, respiratory analeptics, control blood gases and electrolytes. Rinse the stomach with subsequent intake of activated charcoal (orally 50-100 g or 0.5-1 g / kg).
Precautions:
1. Tolerance and addiction to the drug may develop already with repeated use.
2. Reduce the dose in elderly patients with hypovolemia while using other narcotic and sedatives.
3. Oxymorphone contains sodium hydrosulfite, which can cause allergic reactions in susceptible individuals.
4. In case of nausea and vomiting, prescribe cerucal or another antiemetic.
5. It is possible to eliminate or prevent constipation by prescribing light laxatives.
6. Tolerance is manifested by reducing the duration of action and increasing the need for a drug. In this case, you can add other narcotic analgesics, NSAIDs or antidepressants, and support treatment with non-drug therapy.
7. Abrupt interruption of opiate intake in patients with physical dependence may manifest symptoms of withdrawal syndrome. In order to avoid withdrawal syndrome, doses should be gradually reduced (for example, reducing the dose by 75% every 2 days). Further treatment is symptomatic.
8. The combination of the drug with other narcotic drugs enhances analgesia.
9. Non-traditional therapy includes percutaneous electrical nerve stimulation and techniques such as thermal and cold applications, ultrasound, massage.
10. Patients should be warned that oxymorphone may inhibit their ability to solve complex tasks that require concentration or physical coordination, such as driving a car or working in heavy industry.
Side effects.
Cardiovascular system: hypotension, bradycardia, fainting.
Respiratory system: respiratory depression.
CNS: sedative effect, drowsiness, euphoria, dysphoria, disorientation.
Kidneys: urinary retention.
Gastrointestinal tract: nausea, vomiting, abdominal pain, constipation, anorexia, hepatic dysfunction.
Eyes: myosis.
Allergic reactions: rash, urticaria, itching of the skin.
Release forms:
candles 5 mg; solution for injection 1 mg /ml, 1.5 mg/ml.